Patient safety in primary care
The NHS Primary Care Patient Safety Strategy was published by NHS England at the end of September 2024.
Primary care – general practice, community pharmacy, optometry and dental services – delivers 90% of NHS interactions, face to face, by phone or online. The overwhelming majority of these are safe, but with between 20,000 and 30,000 incidents of avoidable significant harm identified in general practice in England per year, there is opportunity to continue to improve the safety of care in primary care. We also know that incident data may be an underrepresentation of harm, as incident recording systems are not as well developed in primary care when compared to secondary care.
The NHS Patient Safety Strategy, the first national strategy for improving patient safety, applies to all sectors. However, NHSE recognised it needs more specific interpretation for primary care. This Primary care patient safety strategy describes the national and local commitments to improve patient safety in primary care, supporting all areas in this sector to fully implement the NHS Patient Safety Strategy.
It focuses on:
- developing a supportive, learning environment and just culture in primary care, with sharing across the system so that the services can continually improve.
- ensuring that the safety and wellbeing of patients and staff is central, and that our approach to managing safety is systematic and based on safety science and systems thinking.
- involving patients in the identification and co-design of primary care patient safety ambitions, opportunities and improvements.
Insight:
Health professional feedback (HPF) via Datix | Learn from patient safety events (LFPSE) | Significant event analysis/ audit (SEA) | Serious incidents (SIs) and the Patient safety incident response framework (PSIRF) | National patient safety alerts (NatPSAs) | GPs and medical examiners (MEs)
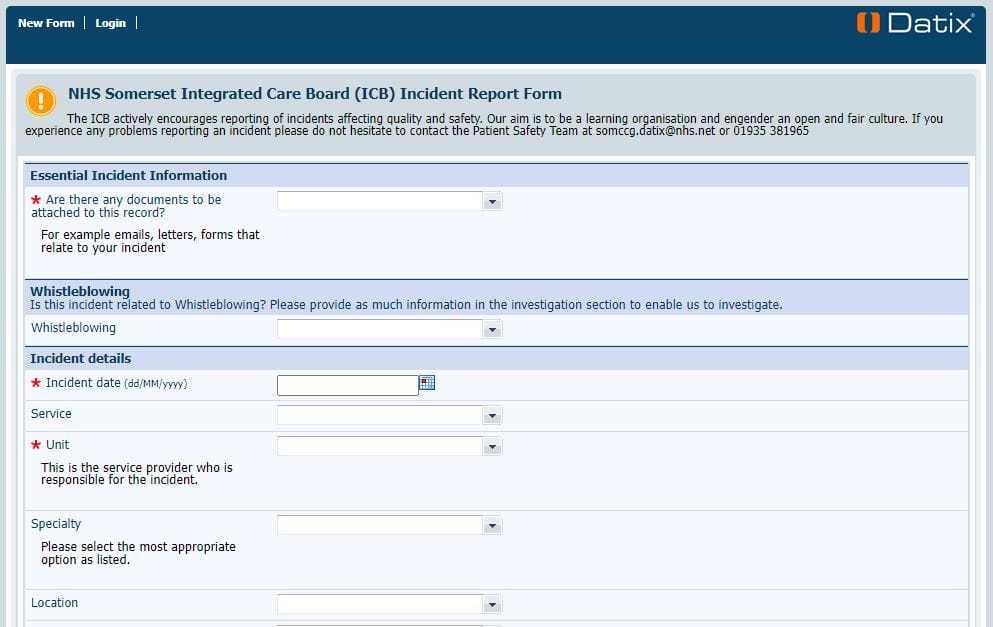
The button on the right takes you to a Datix web form which can be used to report a piece of feedback or an incident your practice may have identified which needs to be shared with another provider for their review and learning. The ICB can support this sharing of information.
We are aware the form needs updating and there is a group looking at this currently. If you cannot find the organisation you're looking for under 'Unit' or your organisation under 'Reporting Service', please try typing 'not' and select the 'Not applicable' option. You can then manually write where you're reporting from and which service is responsible within the 'Description' section.
Where applicable, please ensure an NHS number is included within the 'Protected information' box so that the receiving service can accurately look into the event if needed.
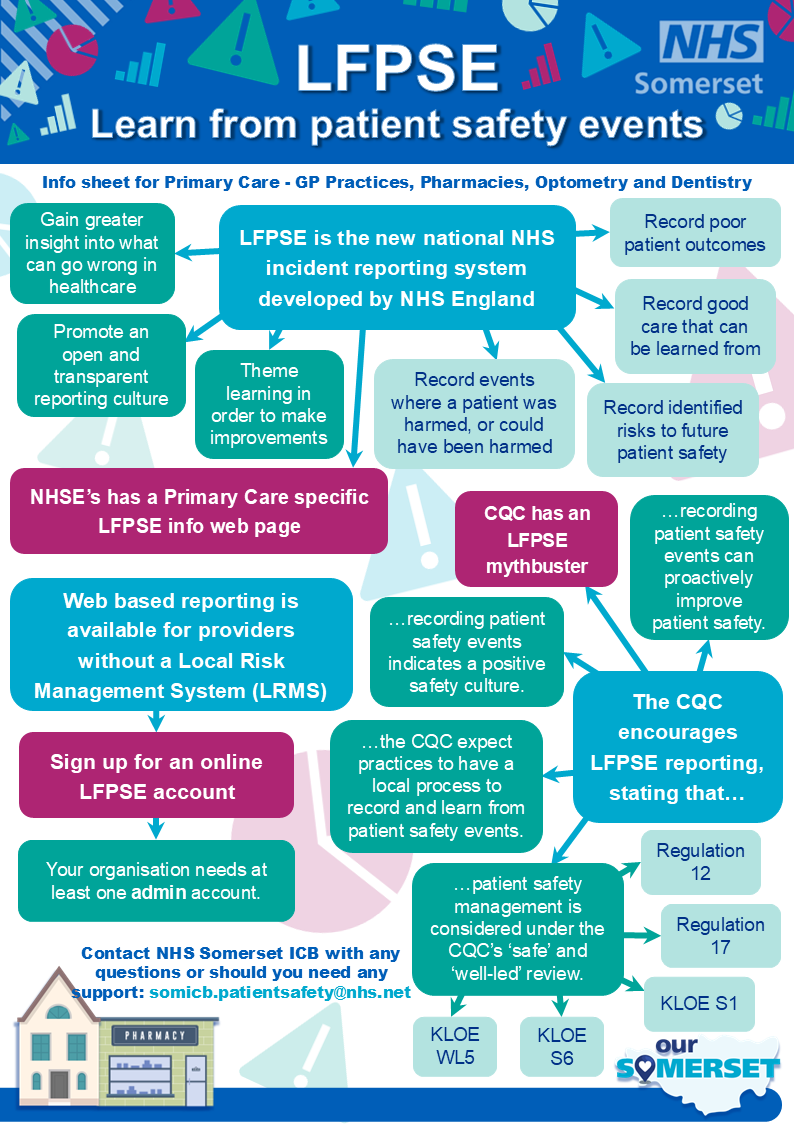
The LFPSE service is a national NHS system set up by the National Patient Safety Team at NHS England, it is free to use and is available online as a web portal, to record information about patient safety events and support the improvement of safety across all care settings.
Recording patient safety events, whether they result in harm or not, provides valuable insight into what can go wrong in health and care, and the reasons why. It also acts as a basis for a positive safety culture, demonstrating an openness and transparency within the organisation to report and learn from patient safety events.
All healthcare staff in England, including those working in primary care, are encouraged to use the system to record any events where:
- a patient was harmed, or could have been harmed;
- there has been a poor outcome but it is not yet clear whether an incident contributed or not;
- risks to patient safety in the future have been identified;
- good care has been delivered that could be learned from to improve patient safety.
Patient safety events can be recorded by your service about incidents that have happened internally, or those that your service has identified and wants to report to another organisation. Additionally, staff members from other organisations and members of the public will be able to report patient safety concerns directly onto the system about services. To see and respond to these incidents you need to be registered.
LFPSE allows users to access data that has been submitted, to better understand their local recording practices and culture, and to support local safety improvement work.
The LFPSE toolkit we've put together should provide you with all the information you require to start using LFPSE, outlining what LFPSE is, how to register on the system, and the benefits of using it in practice.
After recording your first incident, get in touch with NHS Somerset's patient safety team so that we can offer you support with the system and gather your feedback. Any insights into the positives or negatives of LFPSE will be most welcome to support our rollout to the wider system.
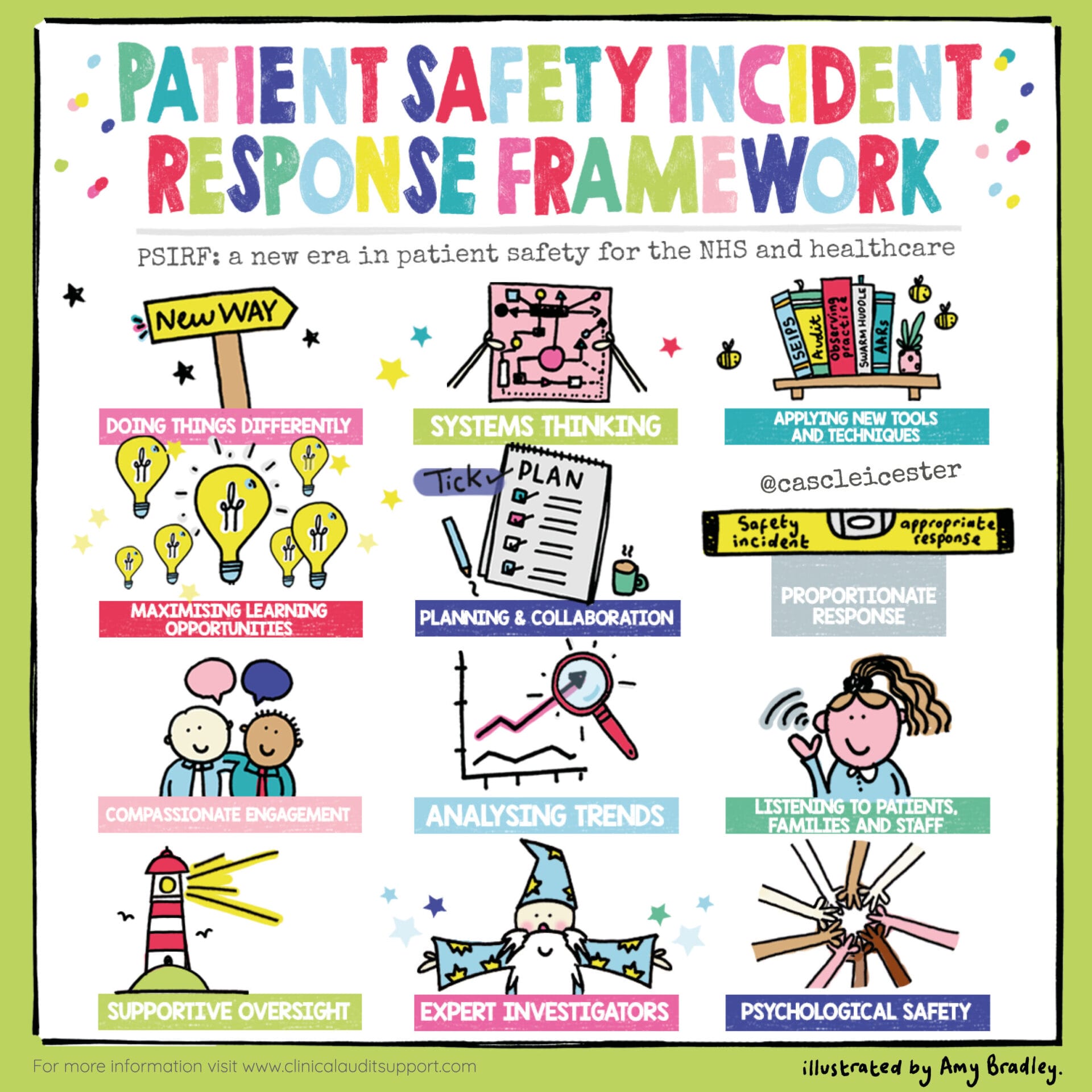
The Patient Safety Incident Response Framework (PSIRF) 2022 is currently being piloted amongst a number of primary care organisations nationally. The learning from this pilot will then help with the wider roll out of PSIRF to the rest of the primary care sector.
Primary care providers are required to work to the Serious Incidents Framework (SIF) 2015 until such a time as their organisation has officially transitioned to PSIRF. The SIF describes the process and procedures to help ensure serious incidents are identified correctly, investigated thoroughly and, most importantly, learned from to prevent the likelihood of similar incidents happening again.
However the PSIRF approach and its principles are highly encouraged by Somerset ICB. PSIRF is all about developing and maintaining effective systems and processes for responding to patient safety incidents for the purpose of learning and improving patient safety. Its four principles are as follows:
- Compassionate engagement and meaningful involvement of those affected by patient safety incidents.
- Application of a range of system-based approaches to learning from patient safety incidents.
- Considered and proportionate responses to patient safety incidents.
- Supportive oversight focused on strengthening response system functioning and improvement.
Should your primary care organisation identify a patient safety event that you wish to review under the PSIRF principles please do get in touch with our team who may be able to support with tools, resources and methodology: somicb.patientsafety@nhs.net.
All patient safety events should be reported to the Learn From Patient Safety Events LFPSE) service (further information can be found further up this page).
Significant event analysis, also known as significant event audit (SEA) is a collective learning technique used to investigate patient safety incidents (circumstances where a patient was or could have been harmed) and other quality of care issues.
Once identified, all significant events should be reported to the ICB via: somicb.patientsafety@nhs.net. The NHS Somerset Patient Safety team will then be in contact to discuss any support that may be needed.

All providers commissioned under the NHS Standard Contract must be registered with the Central Alerting System to receive and appropriately respond to the actions published in patient safety alerts.
Notifications may also be received from the Medicines & Healthcare products Regulatory Agency (MHRA). The majority of those from the MHRA will be aimed at pharmacies and dispensing GP practices where action will be required in relation to medication safety.
As of 09 September 2024, all deaths in any health setting that are not investigated by a coroner will be reviewed by an NHS medical examiner. Medical practitioners are now able to complete a medical certificate of cause of death (MCCD) if they attended the deceased in their lifetime.
As all deaths not investigated by a coroner must be independently reviewed by a medical examiner, all healthcare providers including GP practices and independent healthcare providers employing medical practitioners who complete MCCDs must work with an NHS medical examiner office.