For more information on supporting patients with a history of oestrogen sensitive cancer, you can seek advice from the Somerset Menopause service by writing to them.
See the main Menopause and HRT page and scroll to “Breast Cancer History or at Risk of Breast Cancer” information for more information and links.
Patients will all need self-care advice on vulval care, vaginal moisturisers as needed and vaginal lubricants during sex.
The advice on the use of local (vaginal) oestrogen varies depending on the type of breast cancer and current adjuvant endocrine therapy (tamoxifen or aromatase inhibitor).
Patients who can usually be prescribed local oestrogen:
- Patients taking tamoxifen
- Patients who have finished or stopped their adjuvant endocrine treatment (usually 5 - 10 years post initial treatment)
- Patients with hormone receptor negative breast cancer
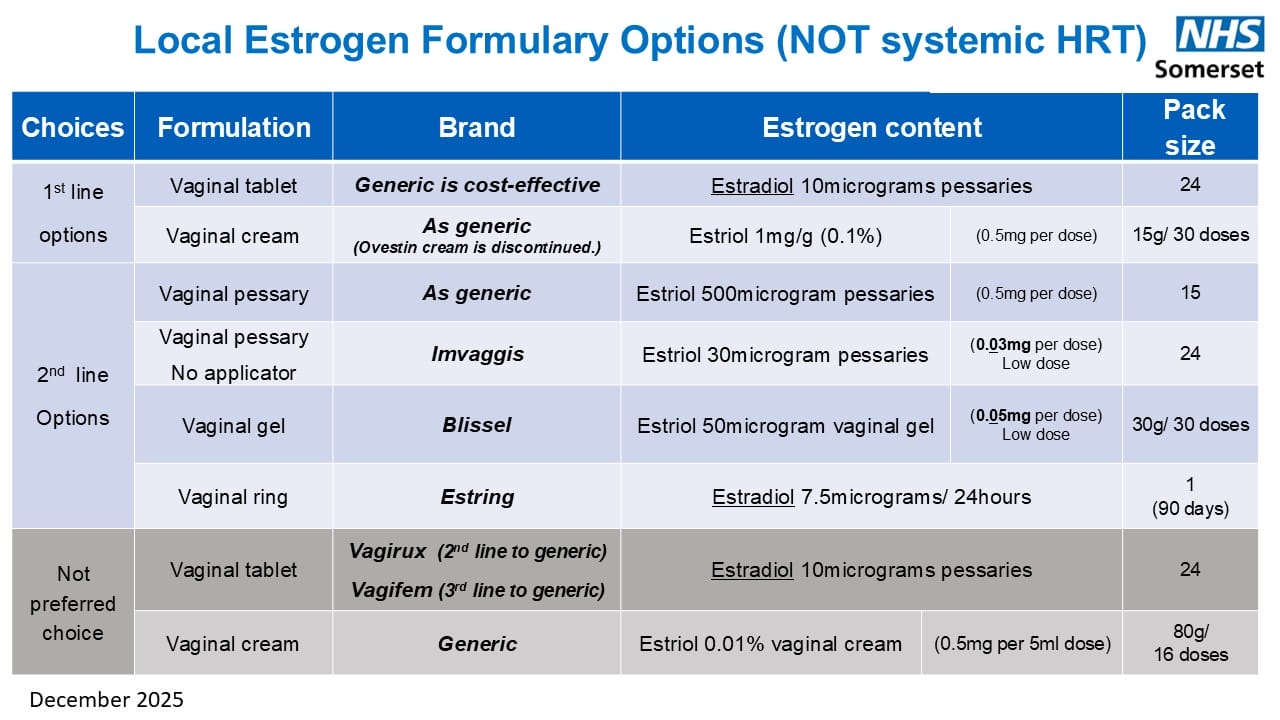
The ultra-low dose estriol products (rather than estradiol) are recommended as first line for these patients i.e. Imvaggis pessaries or Blissel gel.
Patients Taking Aromatase Inhibitors
Unfortunately, this group can get severe GSM symptoms, the use of local oestrogen is controversial as the limited studies we have show conflicting results.
The patient needs to discuss all their treatment options with their oncology team, this may include ultra-low dose local estrogen or a change to tamoxifen if indicated. The Somerset NHS Menopause Service can also provide guidance.
It is recommended that patients on aromatase inhibitors are prescribed YES vaginal moisturiser, to be used daily from the start of their treatment with their aromatase inhibitor. This product is non-formulary for self-limiting conditions but is prescribable for cancer patients who need daily treatment of these products. YES products are considered the preferred choice in this situation.