Patient Safety - home page

Patient safety is the guiding principle for all who work in the NHS, the first and most important lesson staff should learn is how to act safely. The Patient Safety Syllabus applies to all NHS employees. The syllabus sets out the national approach to patient safety, emphasising being proactive in identifying risks to safe care while also including systems thinking and human factors.
The training has five levels, the first level, Essentials for patient safety, is the starting point and all NHS staff are encouraged to complete it.
Patient Safety Specialists are required to complete the training up to Level 4.
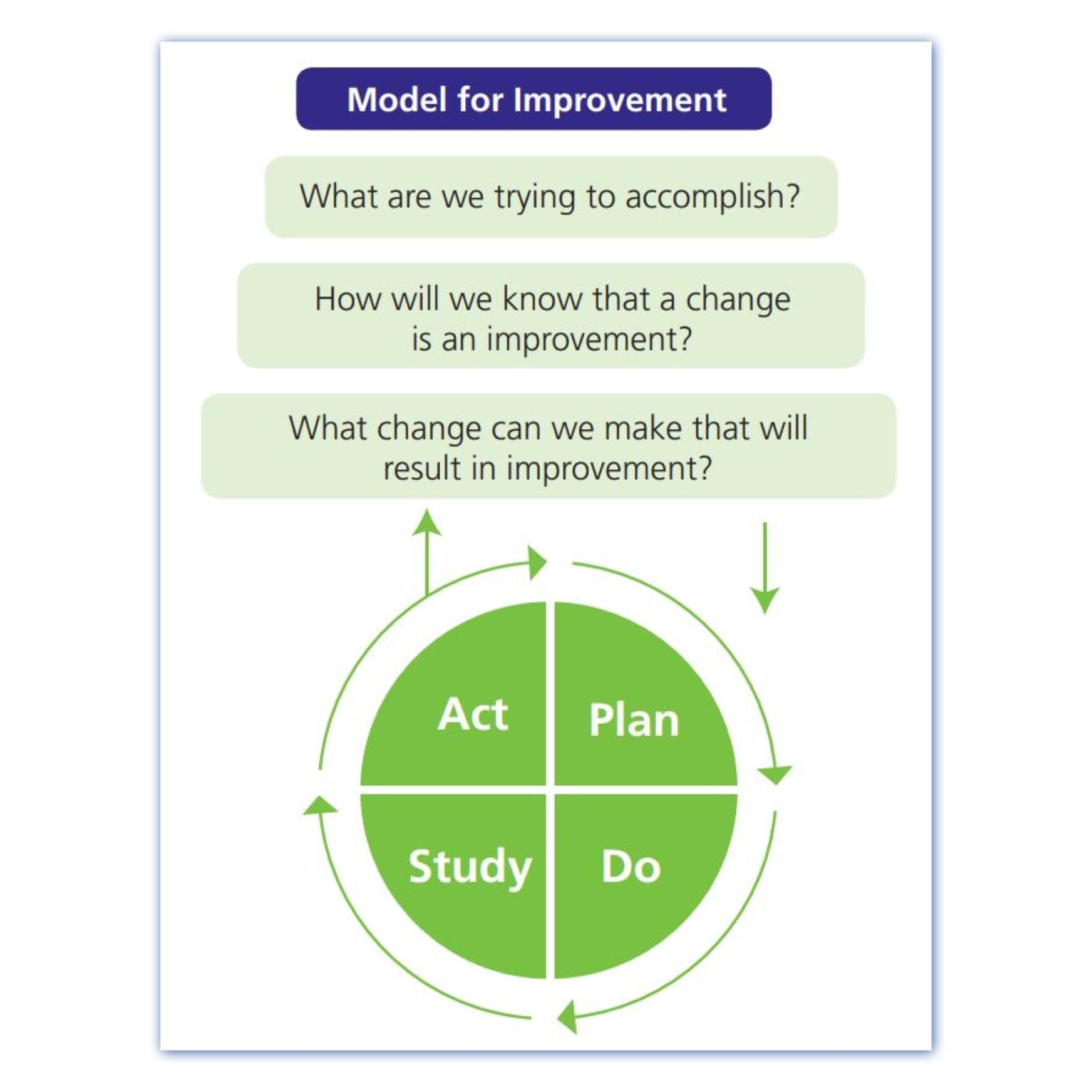
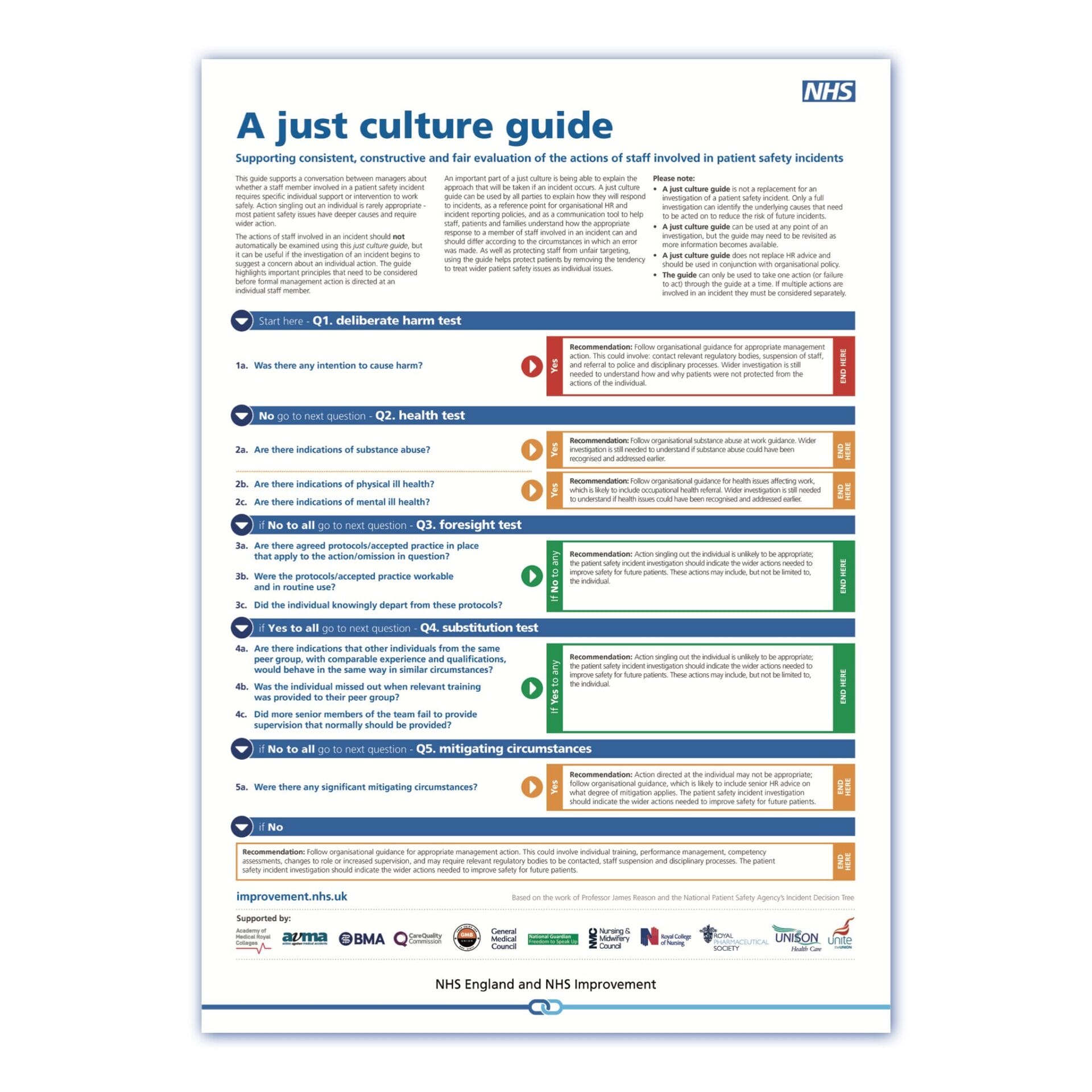
The Patient Safety Incident Response Framework (PSIRF) 2022 replaces the Serious Incident Framework (SIF) 2015. PSIRF shifts how the NHS responds to patient safety events and is a key part of the NHS Patient Safety Strategy. It supports the development and maintenance of an effective patient safety incident response system that integrates four key aims:
- compassionate engagement and involvement of those affected by patient safety events;
- application of a range of system-based approaches to learning from patient safety events;
- considered and proportionate responses to patient safety events;
- and supportive oversight focused on strengthening response system functioning and improvement.
Alongside the PSIRF sits the Learn From Patient Safety Events (LFPSE) service which is the new national NHS service for the recording and analysis of patient safety events. LFPSE is now in use across the NHS, and organisations have switched to recording patient safety events onto the new LFPSE service using LFPSE-compliant local risk management systems LRMS, rather than the National Reporting and Learning System (NRLS) which was decommissioned on 30 June 2024. The Strategic Executive Information System (StEIS, previously used to report serious incidents) is still in use while the next version of LFPSE is rolled out to replace it.
Providers transition from working under the SIF to the PSIRF once their Patient Safety Incident Response Policy and Patient Safety Incident Response Plan (PSIRP) are reviewed and agreed by their lead/coordinating ICB, and subsequently published on their website.
After PSIRF transition, providers will no longer be required to report incidents which would have previously met the serious incident criteria onto StEIS. Though for the interim, until a provider’s Local Risk Management System (LRMS) is updated to LFPSE taxonomy v6, PSIRF transitioned providers will StEIS report incidents due to follow a full Patient Safety Incident Investigation (PSII) response, in line with guidance from the National Patient Safety Team at NHS England – see here for specific reporting guidance.
The ICB’s responsibility within the patient safety events space has moved away from seeking assurance and quality reviewing providers’ individual incident responses, to instead be that of the following:
- Established roles, responsibilities, and processes for oversight.
- Established mechanisms for escalation of incidents and risks that may require support or action at ICB level.
- Understanding and reviewing providers’ patient safety incident and improvement profiles.
- Working collaboratively with providers if incident intelligence demonstrates that ongoing improvement work is not having the desired effect, to assess the systems and processes in place and support safety improvement.
- Supporting coordination of multi-agency learning responses.
- Sharing learning and good practice across organisations.
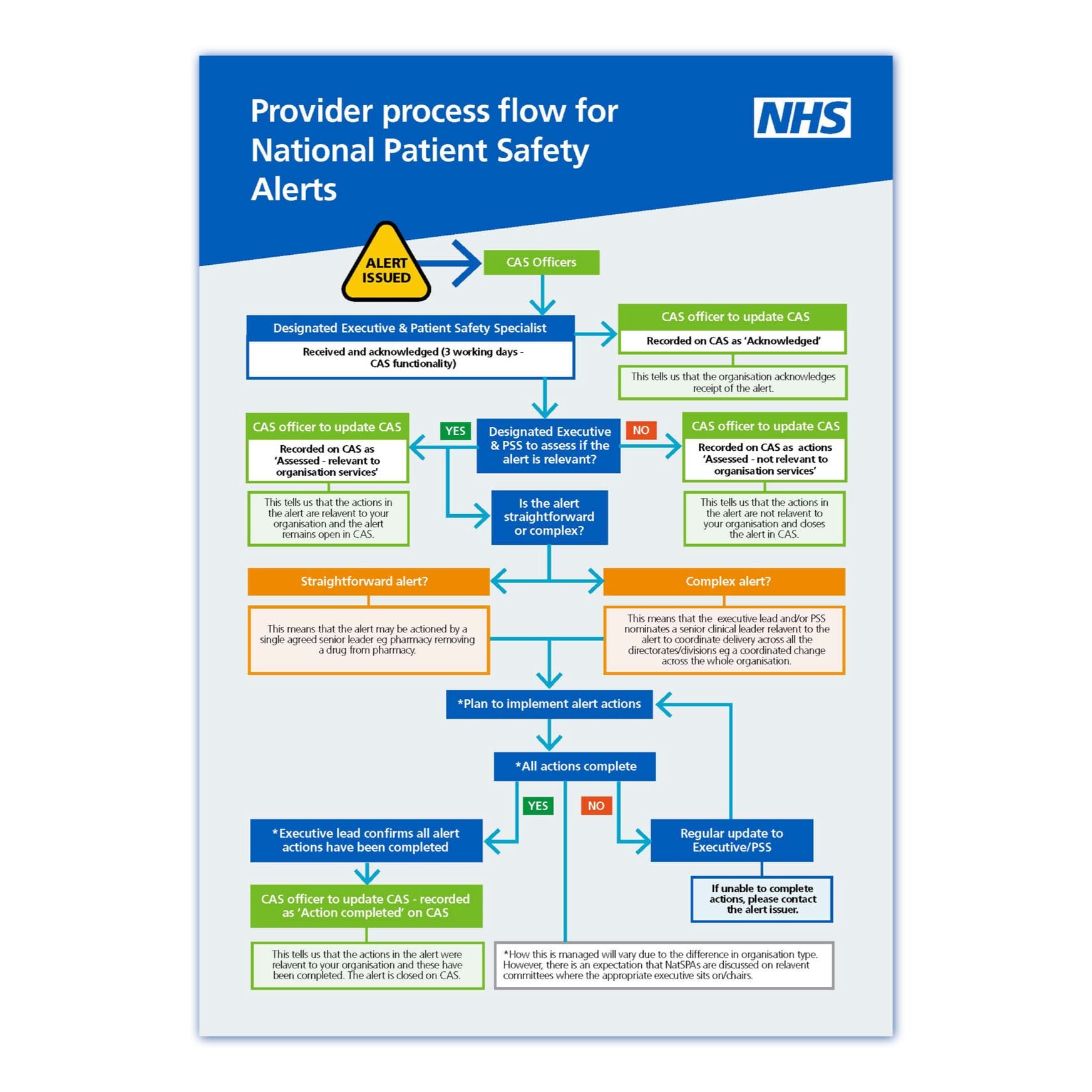
National Patient Safety Alerts (NatPSAs) are alerts issued by the Central Alerting System that require action to be taken by healthcare providers to reduce the risk of death or disability. They are developed from new or under-recognised patient safety issues which are identified through clinical review of incidents or via the national incident reporting service, as well as other sources.
The NHS Patient Safety Strategy recognises the importance of involving patients, their families and carers and other lay people in improving the safety of NHS care, as well as the role that patients and carers can have as partners in their own safety. The Framework for involving patients in patient safety was published in 2021 and is relevant to all NHS trusts and commissioners. It is also useful to other NHS settings, including primary care and community services that are considering how they can involve patients in safety. ICSs should consider how patients can be involved as part of safety governance processes as we develop and mature. The second part of the framework details Patient Safety Partner (PSP) involvement in organisational safety and relates to the role that patients, carers and other lay people can play in supporting and contributing to a healthcare organisation’s governance and management processes for patient safety.
The National Patient Safety Improvement Programmes collectively form the largest safety initiative in the history of the NHS. They support a culture of safety, continuous learning and sustainable improvement across the healthcare system, helping to reduce the risk of harm and make care safer for all. The programmes are delivered by the National Patient Safety Improvement Programmes Team working with the Health Innovation Network’s 15 regionally-based Patient Safety Collaboratives who support Integrated Care Systems (ICSs) and local health providers, to bring about practical improvements to patient safety.
A new statutory Medical Examiner System is being rolled out across England and Wales to provide independent scrutiny of deaths, and to give bereaved people a voice. From 09 September 2024 all deaths in any health setting that are not investigated by a coroner will be reviewed by NHS Medical Examiners. There will be a new medical certificate of cause of death (MCCD) and medical practitioners will be able to complete an MCCD if they attended the deceased in their lifetime.
Our quality assurance and improvement framework 2025-2027 has been published.
This document describes the framework Somerset ICB will adopt to deliver on our statutory duty for quality. It sets out our vision for quality, the application of the National Quality Board guidance, our governance arrangements and our quality priorities.

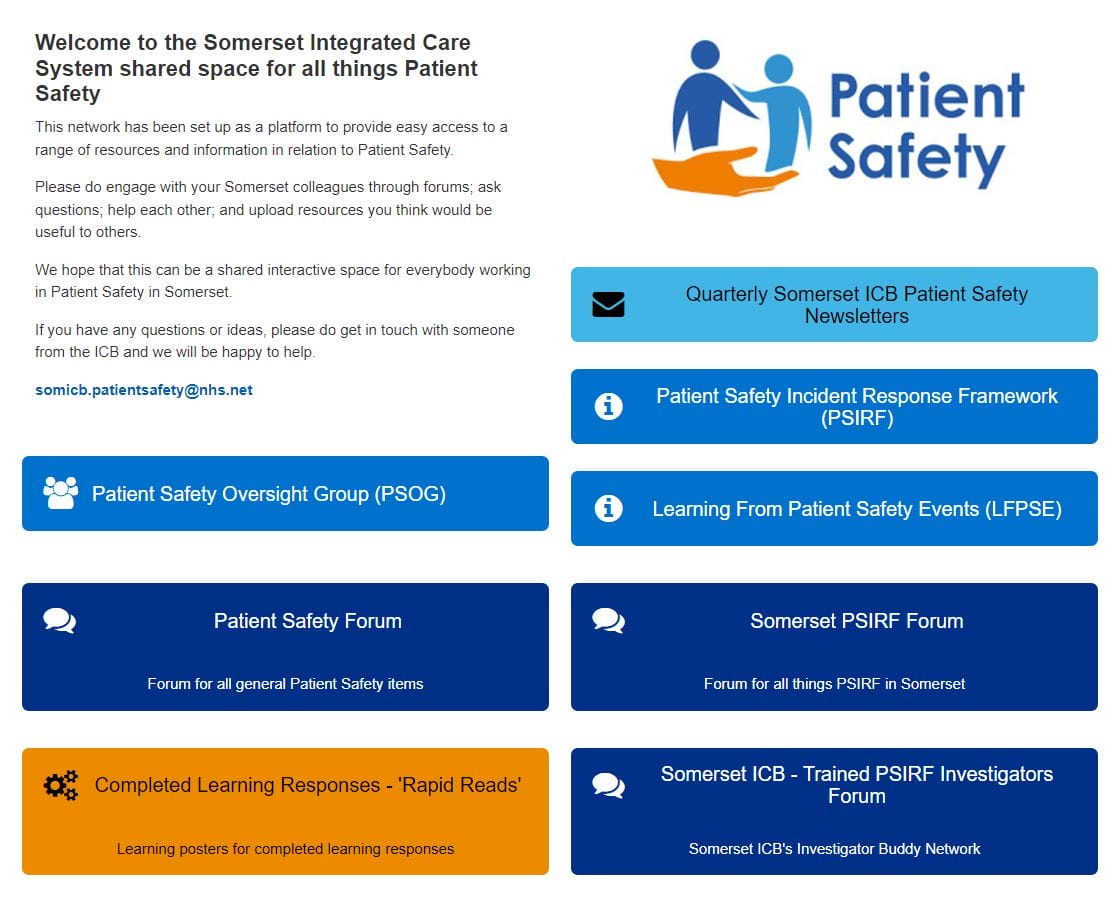
Colleagues across our ICS who work in patient safety are encouraged to join our Somerset Patient Safety Network on the FutureNHS site.
This network has been set up as a platform to provide easy access to a range of resources and information and a way to engage with fellow colleagues through forums.
We hope that this can be a shared interactive space for everybody working in patient safety in Somerset.
If you have any questions or ideas, please do get in touch with someone from the ICB's patient safety team and we will be happy to help where possible.