Medicines Safety
Reducing risk of error and harm.
Prescribing
Patient benefit from medicine safety improvements has resulted in an estimated 518 lives being saved, the prevention of 4,676 severe harms, 24,128 hospital readmissions avoided, and £9.6M avoided costs of admissions due to harm from medicines.

Click here to MHRA website for
- Alerts, recalls and safety information: medicines and medical devices
- Drug Safety Update
- Yellow Card: Report a problem with a medicine or medical device
Clopidogrel and proton pump inhibitors: interaction—updated advice
Citalopram and escitalopram: QT interval prolongation
Emollients and risk of severe and fatal burns: new resources available
Valproate - reproductive risks
Nitrofurantoin: reminder of the risks of pulmonary and hepatic adverse drug reactions
GLP-1 medicines for weight loss and diabetes: what you need to know
See below the growing number of cases of propranolol overdose in patients prescribed for anxiety.
Imogen Heap: Prevention of Future Deaths Report
Joshua Delaney: Prevention of Future Deaths Report
Claire Briggs: Prevention of Future Deaths Report
Aoife McAdam: Prevention of Future Deaths Report
Ania Sohail: Prevention of Future Deaths Report
Charlotte Comer: Prevention of Future Deaths report
Sophie Williams: Prevention of Future Deaths Report

Propranolol prescribed in vulnerable mental health patients search is available via
This will provide list of patients in your practice which would benefit from medication review. These patients have a history of depression, anxiety, self-harm or suicide and prescribed propranolol for anxiety.
Propranolol is not recommended in the treatment of anxiety (NICE).

GP mythbuster 12: Accessing medical records and carrying out clinical searches
Search categories
- Monitoring patients prescribed DMARDs
- Medicines requiring monitoring
- MHRA/Central Alerting System appropriate action in response
- Potential missed diagnosis
- Medicines usage
- Medication review
- Monitoring of high-risk patients with long-term conditions
- We may also look at:
GP mythbuster 91: Patient safety alerts
Practices need systems and processes to disseminate and act on patient safety issues and information. This includes information from external sources that could affect patient safety.
Sources of information include:
- National Patient Safety Alerts.
- Medicines and Healthcare products Regulatory Agency (MHRA) safety notifications (medicines recalls, notifications and devices safety information) alerts.
- UKHSA Urgent Public Health Messages Central Alerting System (CAS) alerts. See CAS Homepage (MHRA).
- Local or national clinical guidance.
- National and local formularies.
- Health Protection Agency alerts.
- MHRA updates

Use the central alerting system to view and search patient safety alerts, important public health messages and other safety critical information and guidance to the NHS and others, including independent providers of health and social care.
Harm from incorrect recording of a penicillin allergy as a penicillamine allergy
Shortage of Antimicrobial Agents Used in Tuberculosis (TB) Treatment
Shortage of bumetanide 1mg tablets
Shortage of Pancreatic enzyme replacement therapy (PERT) - Additional actions
Shortage of Kay-Cee-L (potassium chloride 375mg/5ml) (potassium chloride 5mmol/5ml) syrup
Shortage of Pancreatic enzyme replacement therapy (PERT)
Shortage of salbutamol 2.5mg/2.5ml and 5mg/2.5ml nebuliser liquid unit dose vials
Shortage of GLP-1 receptor agonists (GLP-1 RA) update
Potential for inappropriate dosing of insulin when switching insulin degludec (Tresiba) products
Potent synthetic opioids implicated in heroin overdoses and deaths

Potential under-recognised risk of harm from the use of propranolol
Weight-based medication errors in children
Unintentional overdose of paracetamol in adults with low bodyweight
Unintentional overdose of morphine sulfate oral solution
Online prescribing: challenges and opportunities to improve patient safety

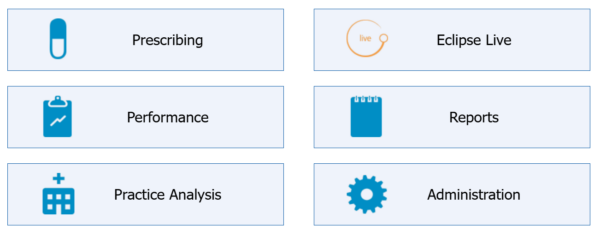
A means of risk stratifying patients which allows medicines optimisation to reduce risk and improve patient outcomes.
For practice level data Eclipse is the best risk reduction tool available.
Patient safety – Preventing harm and avoidable hospital admissions.
Quality improvement tool – Identify trends and focus on prevention.
Audit tool – Provides assurance that medicines safety is being reviewed regularly.
New user requests can be made via support@prescribingservices.org
For practice level access, practice manager will need to authorise request.
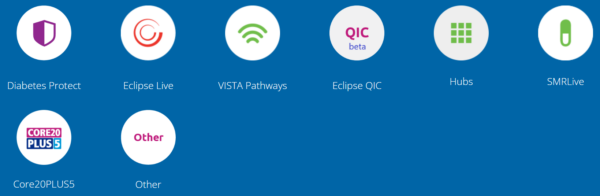
- Diabetes protect
- Eclipse live (red, amber & blue alerts)
- Vista pathways
- QIC (QOF, IIF & CQC)
- Hubs (eGFR, Haemoglobin, BP, TSH, Metabolic score/BMI)
- SMR
- Core 20 PLUS 5
- Eclipse live (local searches)
- Reports (savings switches)



University of Liverpool Hepatitis Drug Interactions
University of Liverpool HIV Drug Interactions

SPS: Understanding drug interactions
- Considerations and interactions with GLP-1 receptor agonists
- Managing interactions with methotrexate
- Managing interactions with direct oral anticoagulants (DOACs)
- Using contraception with enzyme-inducing medicines
- Managing interactions between macrolides and statins
- Considering drug interactions with smoking
- Using clopidogrel with proton pump inhibitors (PPIs)
- Using warfarin with proton pump inhibitors (PPIs)
- Using folic acid and phenytoin safely
- Using bisphosphonates with proton pump inhibitors (PPIs)
- Managing interactions between medicines and enteral feeds
- Identifying risk factors for developing a long QT interval
NHS Somerset Joint Formulary - oral anticoagulants
- Before initiating anticoagulant - baseline clotting screening, body weight, full blood count, liver function tests, serum creatinine, urea and electrolytes are required.
- Check dose - calculate CrCl (Cockcroft and Gault is recommended) and ensure the right dose is prescribed to avoid harm (increased risk of bleeding) and ensure efficacy (preventing thrombus).
- Counsel patient on the signs and symptoms of bleeding - bruising or bleeding under the skin, tar-coloured stools, blood in urine, nose-bleed, dizziness, tiredness, paleness or weakness, sudden severe headache, coughing up blood or vomiting blood and advise them to seek medical attention immediately and to carry alert card at all times.
- Monitor full blood count, liver function tests, urea and electrolytes and serum creatinine annually or more frequently if required depending on patient factors, such as renal impairment, age, and comorbidities.
- NHS Somerset recommends people prescribed long term NSAIDs, antiplatelet or an anticoagulant should be considered for co-prescribing with a Proton Pump Inhibitor to reduce GI bleed risk.
- Bleeding may be present if there is an unexplained fall in haemoglobin - review patient immediately.
- Regularly review anticoagulant related Eclipse live red and amber alerts and action to prevent harm and hospital admissions.

This year will be the tenth annual #MedSafetyWeek social media campaign and it will take place on 3 to 9 November 2025. The theme will be ‘we can all help make medicines safer’.

17 September 2025: “Safe care for every newborn and every child”
A single safety incident can have lifelong consequences for a child’s health and development. That’s why World Patient Safety Day 2025 is dedicated to ensuring safe care for every newborn and child, with a special focus on those from birth to nine years old. This year’s slogan, “Patient safety from the start!”, emphasizes the urgent need to act early and consistently to prevent harm throughout childhood, and yield benefits across the life course.
The Medicines Safety Officer for NHS Somerset ICB is Esther Kubiak esther.kubiak@nhs.net

Includes links to MHRA guidance, regulatory requirements and local searches to facilitate identification of your patients in practice. Code patient when Pregnancy Prevention Programme is completed.
- Risk acknowledgement forms
- Patient guide/cards
- Health professionals guide
- Whole pack dispensing/stickers
Information about the reproductive risks of taking valproate medicines and the measures in place to reduce potential harm.
To support the implementation of these measures for valproate, the following safety and educational materials are available:
- Patient guides for female and male patients: Provides those taking valproate (or their parent, caregiver, or responsible person) with information on the risks of valproate in pregnancy and the risks to male patients and what they need to do.
- Healthcare professionals Guide: Provides updated information for healthcare professionals on the risks of valproate in pregnancy and the risks for male patients, the new conditions for valproate prescribing and key points for patient discussions.
- Annual Risk Acknowledgement Form: For female patients under 55 years starting valproate and at annual review. Used to support and record the discussion between the patient and specialist prescriber on the risks associated with valproate in pregnancy and to record the decision of the countersigning specialist. At subsequent annual reviews only one specialist is required.
- Male Risk Acknowledgement Form: Used to support and record the discussion between the patient and specialist prescriber of the risks associated with valproate in males under 55 years when starting treatment with valproate and to record the decision of the countersigning specialist. This is only to be completed at initiation of valproate.
- Patient Card: Provides key information for female patients receiving valproate on contraception and pregnancy prevention and precautionary advice for males and their female partner to use effective contraception.
- Pharmacy Poster: Provides important actions for pharmacists dispensing valproate to patients.
Rules introduced in 2023 to ensure all patients receive the whole pack of valproate with the warnings on the box.

Search - Patient Female aged 12-55 prescribed valproate/valproic
Will need to refer patient to SFT specialists to complete Pregnancy Prevention programme.
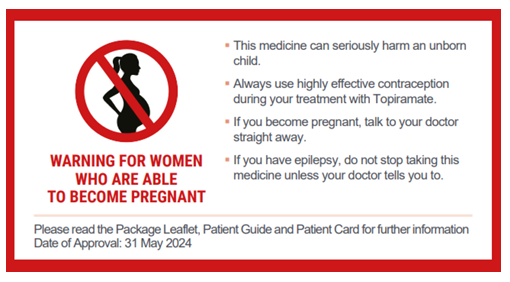
Topiramate is now contraindicated in pregnancy and in women of childbearing potential unless the conditions of a Pregnancy Prevention Programme are fulfilled.
Patient Guide for Migraine and Epilepsy - to be provided to all girls and women of childbearing potential who are started on, or continue to use, topiramate-containing medicines
Guide for Healthcare Professionals for Migraine and Epilepsy
Risk Awareness Form for Migraine and Epilepsy - for the healthcare professional and the patient (or responsible person) to sign at initiation of treatment with topiramate and at annual treatment reviews. The patient should receive a copy of this form, a copy should be filed in the patient’s medical notes, and, if necessary, a copy sent to the patient’s GP
Patient Card - to be given by pharmacists to all female patients who are dispensed topiramate to inform them of the risks

Search - Patient Female 12-55 prescribed topiramate
Will need to refer patient to SFT specialists to complete Pregnancy Prevention programme for <18 and adults for epilepsy/tremor and mental health indication.
Health professionals in general practice can complete Pregnancy Prevention Programme for adult patients with migraine or neuropathic pain:
- For any female planning pregnancy, advise tapering dose and stopping. Usual target dose is 100mg BD, taper weekly to 75mg BD, then 50mg BD, then 25mg BD then stop.
- If patient is pregnant, Topiramate can be stopped abruptly and symptoms managed with analgesia.
- all patients must be counselled about the benefits and risks of treatment before isotretinoin is prescribed, including possible mental health and sexual function side effects; we also ask the referrer (usually the GP) to provide information about isotretinoin to the patient and provide counselling (where possible) regarding the benefits and risks of isotretinoin treatment
- isotretinoin, as well as all of the oral retinoid medicines (including acitretin and alitretinoin), are teratogenic; all patients of childbearing potential must be entered into the Pregnancy Prevention Programme
- prescribers should assess patients’ mental health before prescribing isotretinoin including the use of patient-reported outcome measures
- ask patients about any sexual function concerns before prescribing isotretinoin
- give the patient sufficient time to consider, reflect and ask questions before starting isotretinoin treatment
- use the new regulatory risk minimisation materials with all patients: Acknowledgement of Risk Form, Patient Reminder Card, Pharmacist Checklist
- the Lead Prescriber, who initiates isotretinoin treatment, must have expertise in the use of systemic retinoids for the treatment of severe acne and a full understanding of the risks of isotretinoin therapy and monitoring requirements
- initiation of isotretinoin treatment in patients under 18 years of age now requires agreement by 2 independent healthcare professionals that there is no other appropriate effective treatment before it is prescribed. This means that isotretinoin should only be prescribed for severe acne that is resistant to adequate courses of standard therapy
- review patients approximately 1 month after initiation of treatment in a face-to-face (in-person) appointment
- monitor patients for side effects including mental health and sexual function side effects at each follow up appointment including objective mental health patient reported outcome measures
- any healthcare professional involved in the treatment of patients with acne, particularly prescribers of isotretinoin, should review the full details of the new requirements in the Report of The Commission on Human Medicines Isotretinoin Implementation Advisory Expert Working Group
- report suspected adverse drug reactions associated with isotretinoin on a Yellow Card