Cardiovascular System
Prescribing Guidelines by Clinical Area
Cardiovascular disease (CVD) remains a leading cause of morbidity and mortality, yet significant variation persists in outcomes, treatment gaps, and access to evidence-based interventions.
This webpage brings together local, regional, and national CVD data to support a clearer understanding of population need, unwarranted variation, and health inequalities. It enables readers to explore treatment gaps and equity of access across key CVD pathways, while signposting best-practice guidance for the prevention and management of atrial fibrillation, lipid disorders, and hypertension. The aim is to support informed, data-driven action to improve cardiovascular outcomes and reduce inequalities across populations.
Cardiac Data Hub - Link to data sources to support local quality improvement
- CVDPREVENT Quality Improvement Tool - The Cardiovascular Disease Prevention Audit (CVDPREVENT) is a nationwide primary care audit that automatically extracts routinely recorded GP data. It offers open access to this information, presenting clear and actionable insights to support those working to improve cardiovascular health across England.
- Cardiovascular Disease | Fingertips | Department of Health and Social Care - The Fingertips public health data for CVD – Coronary Heart Disease (CHD) includes a range of QOF indicators covering patients with stroke, heart failure, atrial fibrillation and a range of QOF indicators on high risk factors for CVD, including hypertension, obesity, smoking.
- Excess mortality in England - The Public Health Analysis Unit within the Office for Health Improvement and Disparities (OHID) produces the Excess Mortality in England: Weekly Reports. These reports outline how weekly and cumulative excess deaths in England.
- Insight - Model Health System - The Model Health System is a data-driven improvement tool that enables NHS health systems and trusts to benchmark quality and productivity. It offers insights into cardiovascular disease outcomes and highlights inequalities in access to care pathways. Requires NHS England Application sign in.
- The BHF heart statistics visualised - The British Heart Foundation’s interactive data visualisations are designed to help people better understand the key insights from heart and circulatory disease data.
Diagnosing atrial fibrillation (AF) is a crucial step in stroke prevention. AF may be symptomatic or asymptomatic, and can be persistent or paroxysmal. If atrial fibrillation is suspected, perform manual pulse palpation to check for an irregular pulse. This should be considered for people presenting with any of the following:
- Breathlessness
- Palpitations
- Syncope or dizziness
- Chest discomfort
- Stroke or transient ischaemic attack (TIA)
Perform a 12-lead electrocardiogram (ECG) to make a diagnosis of atrial fibrillation if an irregular pulse is detected in people with suspected atrial fibrillation with or without symptoms.
Once AF is detected starting patients on appropriate anticoagulation is the next key step in effective management. Two-thirds of strokes can be avoided through timely and appropriate initiation of an oral anticoagulant (OAC). Risk stratification and clinical decision-making tools have been developed and validated in order to help:
- Determine an individual’s thromboembolic risk and whether an OAC is clinically indicated.
- Determine how best to mitigate against bleeding complications.
CHA₂DS₂-VASc Score for Atrial Fibrillation Stroke Risk, Calculates stroke risk for patients with atrial fibrillation. CHA₂DS₂-VASc Score for Atrial Fibrillation Stroke Risk
Interpretation and application of the CHA₂DS₂-VASc Score
- Score < 0 men or <1 women= OAC is not recommended.
- Score = 1 men or 2 women= OAC should be considered.
- Score ≥ 2= OAC should be offered.
ORBIT Bleeding Risk Score for Atrial Fibrillation, Predicts bleeding risk in patients on anticoagulation for AF, ORBIT Bleeding Risk Score for Atrial Fibrillation
NICE NG196 suggest the use the ORBIT bleeding risk score because evidence shows that it has a higher accuracy in predicting absolute bleeding risk than other bleeding risk tools.
Provide ongoing monitoring and support to help reduce bleeding risk by addressing factors such as:
- Uncontrolled hypertension
- Poor INR control in patients taking vitamin K antagonists
- Concomitant medicines, including antiplatelets, selective serotonin reuptake inhibitors (SSRIs), and non-steroidal anti-inflammatory drugs (NSAIDs)
- Harmful alcohol use
- Reversible causes of anaemia
Decision support tool: making a decision about further treatment for atrial fibrillation, This decision support tool is to help with decisions about atrial fibrillation. It includes information about the condition and possible treatments. NHS Atrial Fibrillation Decision Tool
A reminder that for DOACs, Apixaban (Twice Daily Regimen) or Rivaroxaban (Once Daily Regimen) are the joint first line DOACs choice for Somerset. See NHS Somerset netFormulary pages for further information.
Optimising ongoing care in atrial fibrillation ensures that patients receive holistic, high-quality management beyond anticoagulation. This includes using the correct dose of anticoagulant, with renal function monitored regularly in line with best practice guidance. Routine follow-up should also focus on modifying bleeding risk factors, managing comorbidities such as hypertension and heart failure, and supporting lifestyle changes - including weight loss and alcohol reduction.
- SPS DOAC Monitoring Advise, using Cockcroft and Gault is recommended for calculating creatinine clearance for DOACs. Estimated glomerular filtration rate can overestimate renal function and increase risk of bleeding events, DOACs (Direct Oral Anticoagulants) monitoring – SPS - Specialist Pharmacy Service – The first stop for professional medicines advice
- Understand and managing DOAC interactions: It is important to understand the risks, mechanisms of interactions and actions to take when prescribing medicines with DOACs. Interactions with DOACs often arise when medicines increase or decrease the activity of CYP450 enzymes or P-gp. See SPS article for further information: Understanding direct oral anticoagulant (DOAC) interactions – SPS - Specialist Pharmacy Service – The first stop for professional medicines advice
Statement 1: Adults with non‑valvular atrial fibrillation and a CHA2DS2-VASC stroke risk score of 2 or above are offered anticoagulation.
Statement 2: Adults with atrial fibrillation are not prescribed aspirin as monotherapy for stroke prevention.
Statement 3: Adults with atrial fibrillation taking a vitamin K antagonist who have poor anticoagulation control have their time in therapeutic range (TTR) recorded at each visit for INR assessment.
Reassess anticoagulation for a person whose anticoagulation is poorly controlled shown by any of the following:
- 2 INR values higher than 5 or 1 INR value higher than 8 within the past 6 months
- 2 INR values less than 1.5 within the past 6 months
- TTR less than 65%.
NHS Somerset recommends people prescribed long term NSAIDs, antiplatelet or an anticoagulant should be considered for co-prescribing with a PPI to reduce GI bleed risk.
See SmPC for licensed doses of proton pump inhibitors used for gastroprotection.
Co-prescription of a PPI drug with DOACS reduces the risk of an upper GI bleed significantly.
The incidence of hospitalization for upper gastrointestinal tract bleeding was lower among patients who were receiving PPI co-therapy – Reference: https://jamanetwork.com/journals/jama/fullarticle/2717474
- Patient Resources
- British Heart Foundation: Understanding Atrial Fibrillation
- West of England AHSN: Overview_of_AF
- Arrhythmia Alliance: Know Your Pulse
- Wessex AHSN: Starting Anticoagulation with Jack | AF Toolkit
- Clinician Resources
- Eclipse VISTA Pathway, NHS Pathways
Identifying and assessing cardiovascular disease risk for people without established cardiovascular disease
- NICE NG 238 recommends prioritising people for primary CVD prevention in primary care by estimating their risk using existing electronic health records before a full formal assessment. Regularly review CVD risk for those over 40 and refer for formal assessment if their estimated 10-year risk is 10% or higher.
- Use the QRISK3 tool to calculate the estimated CVD risk within the next 10 years for people aged between 25 and 84 without CVD. Until electronic clinical systems in which QRISK2 is embedded are updated with QRISK3, it may be necessary to use QRISK2.
- When assessing risk for people taking corticosteroids or atypical antipsychotics or people with systemic lupus erythematosus, migraine, severe mental illness or erectile dysfunction, use QRISK3 (the online version of QRISK3, if necessary) because QRISK2 does not take these risk factors into account and may underestimate the 10-year CVD risk in these populations.
- Do not use a risk assessment tool for people already at high risk of CVD, including those with:
-
- Type 1 diabetes (see section on primary prevention in type 1 diabetes)
- eGFR <60 ml/min/1.73 m² and/or albuminuria (see section on CVD prevention in CKD)
- Familial hypercholesterolaemia or other inherited lipid disorders (see NICE guideline).
Optimising Lifestyle Changes: Before offering statin treatment for primary prevention, discuss the benefits of lifestyle changes and optimise the management of all other modifiable CVD risk factors if possible.
Statin and Pregnancy: Be aware that statins are contraindicated in pregnancy because of the risk to the unborn child of exposure to statins. Provide contraception counselling to patient(s) who are in child potential age as appropriate.
People with and without type 2 diabetes
- Offer atorvastatin 20 mg for the primary prevention of CVD to people who have a 10-year QRISK3 score of 10% or more.
- Do not exclude atorvastatin 20 mg for primary CVD prevention solely because the 10-year QRISK3 score is below 10%, if the person prefers treatment or their risk may be underestimated.
People with type 1 diabetes
Offer atorvastatin 20mg for primary CVD prevention in adults with type 1 diabetes who are over 40, have lived with diabetes for more than 10 years, have established nephropathy, or possess other CVD risk factors.
Lipid target for people taking statins for primary prevention of CVD aim for a greater than 40% reduction in non-HDL cholesterol. Refer to NHS Accelerated Access Collaborative » Summary of national guidance for lipid management for prescribing guidance and care pathway.
In patient(s) with established cardiovascular disease, offer atorvastatin 80 mg to people with CVD regardless of cholesterol level, unless they:
- take medicines with potential interactions
- have a high risk of adverse effects
- prefer a lower dose
Do not delay statin treatment for secondary prevention of CVD but discuss lifestyle changes at the same time if appropriate
Lipid target for people taking lipid-lowering treatments for secondary prevention of CVD, aim for low-density lipoprotein (LDL) cholesterol levels of 2.0 mmol per litre or less, or non-HDL cholesterol levels of 2.6 mmol per litre or less.
Refer to NHS Accelerated Access Collaborative » Summary of national guidance for lipid management for prescribing guidance and optimising care pathway.
- Offer atorvastatin 20 mg for the primary or secondary prevention of CVD to people with CKD.
- If lipid targets for primary or secondary CVD prevention are not achieved:
- If eGFR is ≥30 ml/min/1.73 m², increase the atorvastatin dose.
- If eGFR is <30 ml/min/1.73 m², agree any dose increase with a renal specialist.
Key messages adapted from the National Lipid Management Webinar - highlighting common myths and misconceptions around statins and lipid-lowering therapies:
Misconception: “My patient thinks lifestyle is enough!”
Fact: Lifestyle change is a fundamental part of managing CVD risk, and some other elements can impact on cholesterol levels.
Lifestyle change is a fundamental part of managing CVD risk, and some elements can impact on cholesterol levels:
- Smoking cessation
- Weight loss if overweight or obese
- Physical activity
- Dietary modification
- Alcohol moderation
However, we also noted that only ~20% of circulating cholesterol comes from dietary sources. The liver manufactures most of the cholesterol in the body.
NICE 2023 Guidance:
- Primary Prevention: "Offer people the opportunity to have their risk of CVD assessed again after they have tried to change their lifestyle."
- Secondary Prevention: "Do not delay statin treatment for secondary prevention of CVD, but discuss lifestyle changes at the same time if appropriate."
Misconception: “My patient can’t tolerate statins”
Fact: While statin intolerance is a common concern, evidence suggests the true prevalence is often overestimated.
Meta-analysis - Prevalence of statin intolerance: a meta-analysis (European Heart Journal, Bytyci I et al., 2022):
The study reviewed over 176 individual studies involving more than 4 million patients and found that the overall prevalence of statin intolerance was approximately 9.1%, based on international definitions. [https://doi.org/10.1093/eurheartj/ehac015]
NHSE Statin Intolerance Pathway. 2024: Provides a structured approach to assessment and management, available at: https://www.england.nhs.uk/aac/wp-content/uploads/sites/50/2020/04/statin-intolerance-pathway-v2.pdf.
Misconception : “My patient is too old!”
Fact : Evidence shows that lipid-lowering therapies are effective in older adults, including those aged 75 and above.
Meta-analysis – Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials (Lancet, Gencer, B. et al. 2020) indicates:
- Benefits of LDL cholesterol reduction in older adults are comparable to those seen in younger patients.
- In patients aged 75 and over, each 1 mmol/L reduction in LDL-C results in a 26% reduction in major vascular events is observed.
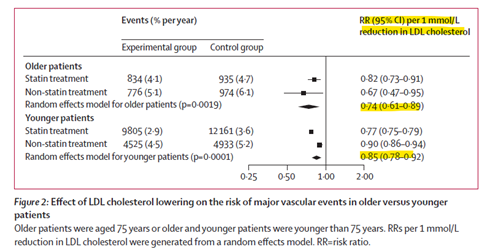
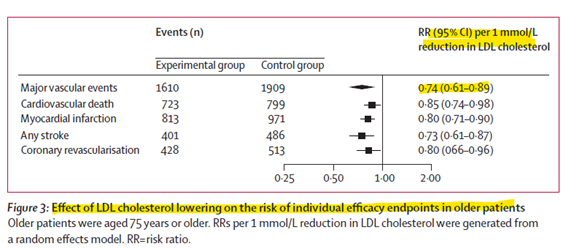
(Result table reference from: Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials - The Lancet)
However, treatment should always be person-centred and guided by individual clinical factors such as comorbidities, polypharmacy, frailty, and palliative care status – not age alone.
- NICE Patient Decision Aids: CG181 Patient decision aid on should I take a statin?
- NHSE Summary of national guidance for lipid management: NHS Accelerated Access Collaborative » Summary of national guidance for lipid management
- NHSE Statin Intolerance Pathway: NHS Accelerated Access Collaborative » Statin intolerance pathway
- NICE [NG238]: Overview | Cardiovascular disease: risk assessment and reduction, including lipid modification | Guidance | NICE
- Eclipse VISTA Pathway – Lipids Optimisation Modules: NHS Pathways
- UCL EMIS Search and Risk stratification tool – Cholesterol: UCLPartners Tools
- Statin interactions from Drug Safety Update: Statins: interactions, and updated advice for atorvastatin - GOV.UK
If clinic blood pressure is between 140/90 mmHg and 180/120 mmHg, offer ambulatory blood pressure monitoring (ABPM) to confirm the diagnosis of hypertension.
If ABPM is unsuitable or the person is unable to tolerate it, offer home blood pressure monitoring (HBPM) to confirm the diagnosis of hypertension.
Confirm diagnosis of hypertension in people with a:
- clinic blood pressure of 140/90 mmHg or higher and
- ABPM daytime average or HBPM average of 135/85 mmHg or higher.
If not diagnosed, repeat at least every 5 years or more frequently if near threshold.
For people with type 2 diabetes, measure BP annually if not previously diagnosed
- Estimate cardiovascular risk in line with the recommendations on identifying and assessing cardiovascular disease risk in NICE's guideline on cardiovascular disease.
- Guidance on the early identification and management of chronic kidney disease, see NICE's guideline on chronic kidney disease.
Coming soon
|
Hypertension |
Clinic Blood Pressure |
ABPM/HBPM Average |
|
Stage 1 |
140/90 mmHg to 159/99 mmHg |
135/85 mmHg to 149/94 mmHg |
|
Stage 2 |
160/100 mmHg to 180/120 mmHg |
150/95 mmHg or higher |
|
Stage 3 or Severe hypertension |
180 mmHg or higher or clinic diastolic blood pressure of 120 mmHg or higher. |
N/A |
Ref: Recommendations | Hypertension in adults: diagnosis and management | Guidance | NICE
When to start drugs
- Offer antihypertensive drug treatment in addition to lifestyle advice to adults of any age with persistent stage 2 hypertension. Use clinical judgement for people of any age with frailty or multimorbidity
- Consider antihypertensive drug treatment in addition to lifestyle advice for adults aged under 60 with stage 1 hypertension and an estimated 10‑year risk below 10%.
- Consider antihypertensive drug treatment in addition to lifestyle advice for people aged over 80 with stage 1 hypertension if their clinic blood pressure is over 150/90 mmHg. Use clinical judgement for people with frailty or multimorbidity.
- People under 40 with hypertension: consider specialist evaluation for secondary causes.
See NICE NG136 table 1 for clinic blood pressure targets for people aged under 80 and table 2 for clinic blood pressure targets for people aged 80 and over. The tables cover people with hypertension (with or without type 2 diabetes) as well as people with chronic kidney disease or type 1 diabetes
Refer to the NICE NG136 Hypertension visual summary flowchart on choice of antihypertensive therapy, treatment monitoring, and blood pressure targets to guide pharmacological management
Please also refer to the NHS Somerset Formulary for formulary drug choices arranged by mode of action.
(Ref: NICE quality standards | Goals and outcome measures | Hypertension | CKS | NICE)
Statement 1: People with suspected hypertension are offered ambulatory blood pressure monitoring (ABPM) to confirm a diagnosis of hypertension.
Statement 2: People with newly diagnosed hypertension receive investigations for target organ damage within 1 month of diagnosis.
Statement 3: General practices use a systematic strategy to identify adults likely to be at high risk of cardiovascular disease.
Statement 4: People with treated hypertension have a clinic blood pressure target set to below 140/90 mmHg if aged under 80 years, or below 150/90 mmHg if aged 80 years and over.
Statement 5: People with hypertension are offered a review of risk factors for cardiovascular disease annually.
Statement 6: People with resistant hypertension who are receiving 4 antihypertensive drugs and whose blood pressure remains uncontrolled are referred for specialist assessment.
Making decisions together: Shared decision-making between healthcare professional and patient. Tailoring treatment based on individual cardiovascular risk and co-morbidities.
Patient decision aid tool
- Patient decision aid on treatment options for hypertension: NG136 Patient decision aid on how do I control my blood pressure? Lifestyle options and choice of medicines
- Patient decision aid on statin prevention: CG181 Patient decision aid on should I take a statin?
Practical tips for patients on the changes on diet to lower blood pressure, including getting active and keeping to a healthy weight.
- Blood Pressure UK: Healthy eating and blood pressure booklet
- Blood Pressure UK: Healthy eating: The African Caribbean way
- Blood Pressure UK: A South Asian guide to controlling your blood pressure
You can also download this in other languages: Bengali, Gujarati, Hindi, Punjabi and Urdu.


